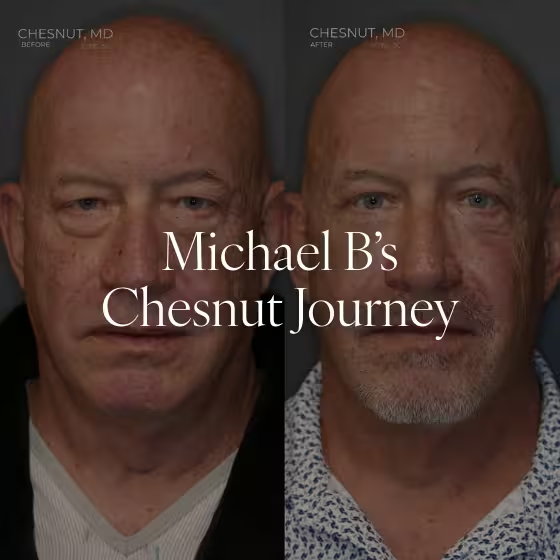
Before & After Gallery
Thank you! Your submission has been received!
Oops! Something went wrong while submitting the form.
Want to learn more about Procedures?
Contact Us
Spokane Clinic (Downstairs)
511 S Pine St Suite A&D
Spokane, WA 99202
Phone: (509) 362-9937
Fax: (844) 961-3417
Fax: (844) 961-3417